In many instances, a woman’s breast size can impede her ability to work, exercise, and even care for her family. Multiple seemingly unrelated areas may experience pain as a result of the weight of breasts that are disproportionately large. After years of wearing “industrial style” support bras, ridges form across the upper shoulders, straining the muscles and frequently causing headaches and neck pain. The delicate skin beneath the breasts is susceptible to inflammation and infection. Chronic lower back pain is a common complaint among women who compensate for their posture by shifting their weight.
Health insurance is one of the most unexpected “obstacles” for women interested in breast reduction surgery.Many of these women are well into the process of preparing for surgery, researching surgeons and enduring (often multiple) consultations and examinations, when they discover that their insurance policy does not cover the necessary procedure.
Reasons For a Breast Reduction
A breast reduction, also known as a reduction mammaplasty, is a surgical procedure that reduces your cup size by removing excess breast tissue, fat, and skin. Due to the negative effects that large breasts can have on their health, many women opt for this surgery. Common health problems that are associated with oversized breasts include:

- Neck pain
- Back pain
- Shoulder pain
- Rounded shoulders (kyphosis)
- Poor posture
- Shoulder grooves from bra straps digging into the skin from inadequate support
- Numbness in the chest, arms, or fingers due to nerve compression
- Breathing problems, specifically while laying down or sleeping
- Skin rashes and infection, typically in the fold beneath breasts
- Migraines
The Cost of Breast Reductions
As of 2023, a reduction mammoplasty can cost between $4,822 and $11,442. This includes the fee for a board-certified plastic surgeon, hospital fees, medical and diagnostic testing, surgical and post-op garments, and medications. This doesn’t include the cost of anesthesia as it can vary greatly depending on the amount used. The surgeon’s fee also varies based on their level of experience and expertise, their surgical techniques, and whether they perform the surgery in an outpatient hospital or a surgical center.
Health Insurance Coverage
As long as the breast reduction surgery meets the criteria for medical necessity, the majority of insurers provide full or partial coverage. Breast reduction is usually considered cosmetic by major insurance companies unless your breasts cause symptoms such as numbness and tingling, ulceration, significant pain, or persistent rashes. In order for an insurer to cover the procedure you have to prove that you have attempted to treat these issues with other means, such as medication or physical therapy. If you can demonstrate that the procedure is medically necessary, the insurer may classify it as reconstructive rather than cosmetic and provide coverage. Health insurance will cover breast reduction if:
- You have breasts that are large enough to be reduced by at least 3 cup sizes.
- The rashes or strap marks cannot be treated properly without the reductions.
- Your breast size was unaffected by documented weight loss.
- Your head, neck, shoulder, or back pain persists despite regular therapy visits.
- The size of your breasts prevents you from exercising and maintaining a healthy body weight.
Like we said above, you have to prove that you have exhausted every other treatment option over a course of 6 to 12 months in an effort to resolve any complications your breast size causes. Your insurance company will only consider covering the breast reduction surgery if you provide documentation of all these health problems and attempted treatments. Even if you are approved you may still have to pay a portion of the surgery, in addition to any deductible or coinsurance associated with the procedure.
Steps To Getting Your Breast Reduction Covered
There are a few steps you may have to go through to make sure your health insurance will cover your breast reduction, including the following:
Meet with your PCP

Understand your benefits
Read through your health insurance benefits of the company’s online resources to learn about your specific level and type of coverage. This will help you find out if you can even get breast reduction surgery covered at all. However, don’t always rely on your own interpretation of your benefits. Reading through will help you gain some understanding about the coverage or what documents you need, but don’t stop there.
Call your insurance company
You can ask your company directly if they will cover the surgery and if pre-approval is necessary for breast reductions. Nextask what kind of documentation you will need to prove medical necessity. You also need to find out if your insurance company will require you to use a plastic surgeon within their network.
Pre-authorization
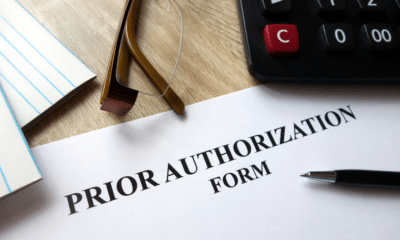
In addition, the majority of plastic surgeons recommend that you have documentation of any complementary and alternative medicine therapies such as acupuncture or chiropractic care. During your initial consultation for breast reduction, your doctor may take photos of your pro-op breasts for insurance purposes. Additionally, they can provide you with a note detailing the symptoms that prompted you to seek breast reduction. All of this documentation will be reviewed by a panel of medical professionals that work for your insurance company. They will evaluate your medical history and determine if breast reduction surgery is medically necessary for your case.
Initial Rejection
According to AARP, up to 14% of all initial insurance claims are denied. However, this doesn’t mean it’s impossible to get coverage. You have the ability to appeal the denial. You do this by having your surgeon write a letter to the insurance company explaining why you qualify for the surgery. It’s also wise to get letters of support from any other medical professionals to strengthen your case.
Authorization
Once your paperwork has been accepted and your insurance company has given its approval, you can go ahead and schedule your breast reduction surgery. The majority of insurance providers will require you to pay a copay for the hospital or medical facility stay. Which can range from $100-$300.
Is A Breast Reduction Ever Automatically Covered?
You won’t need to document a long history of trying to relieve symptoms if your reconstructive surgery is tied to a mastectomy. Which is a breast cancer surgery that removes the entire breast. It is usually offered to women who can’t or doesn’t want to be treated with breast conserving surgery. Which would save most of the breast while removing the cancer cells. It’s also offered to women who have a high risk of getting second breast cancer. In this case, the patient can choose to get a double mastectomy, which will remove both breasts. Now say prior to having your mastectomy you had all of these health issues because you had large breasts. Once you have the mastectomy you are able to get reconstructive breast surgery and your breasts will be a proportional size to your body, therefore alleviating the medical conditions.
Working With EZ
Having breast reduction surgery can significantly improve your quality of life. So, it’s unquestionably worth investigating, especially since some insurance policies will cover the procedure without much hassle. You could enjoy a more active lifestyle with less pain or discomfort. If you are looking for a company that will cover breast reduction surgery, come to EZ. One of our agents will research and compare all available plans within your budget. EZ understands how difficult this pain can be and we want to make getting health insurance one less headache (or backache) for you. Your personal agent will compare all of the quotes in your area. As well as answer any questions you have for free. To get started enter your zip code into the box below for your free instant quotes. Or call one of our licensed agents directly at 877-670-3557.